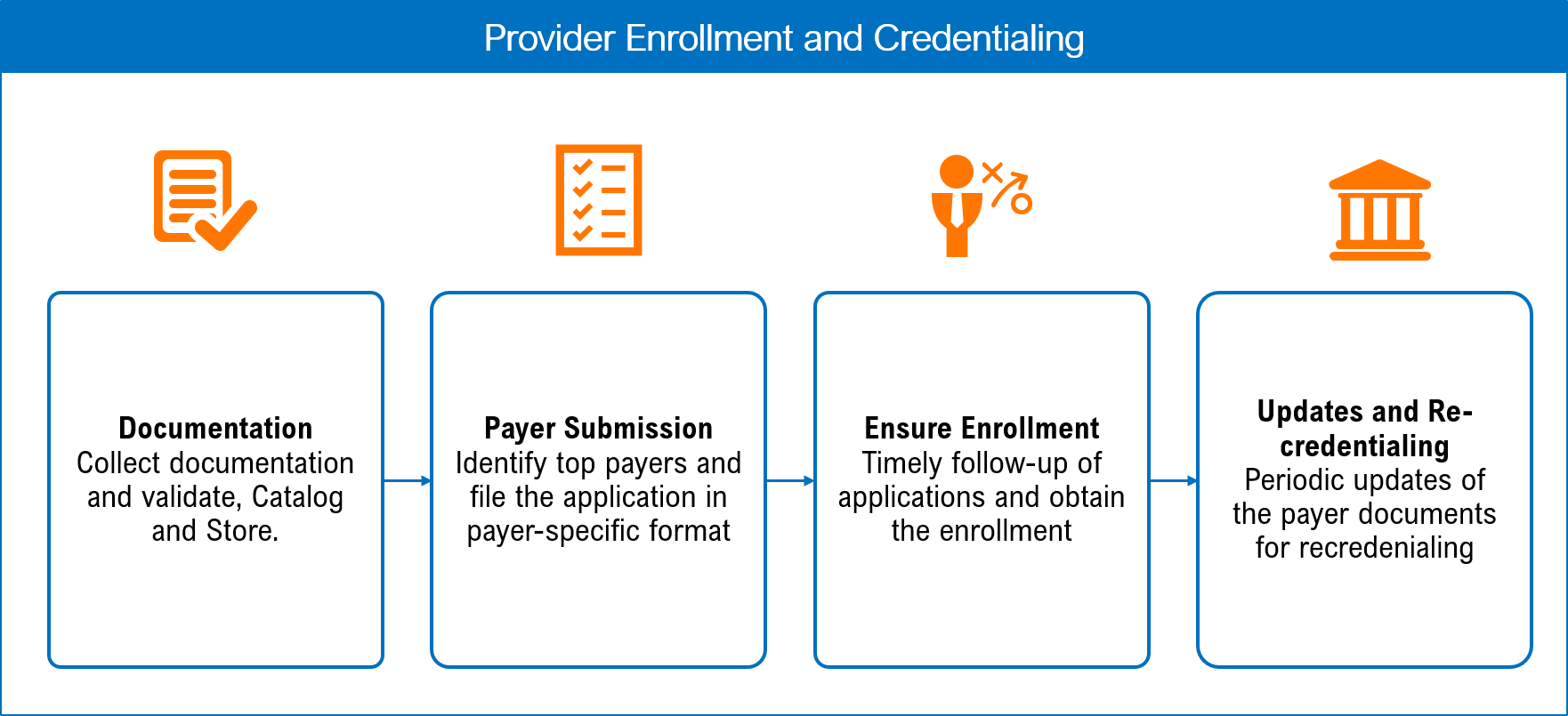
Payer credentialing and contracting process – Yawn! The most boring topic – Yet one of the most important for medical providers. The process is laborious and tedious.
Gathering paperwork, filling out forms, and negotiating is not how most professionals want to spend their time, unless of course they are attorneys or accountants 😉
The process is meant for the payers to “vet” medical providers and make sure they are legit. (Wiki: Credentialing)
The process also allows the provider, to align themselves with different employer groups or accountable health organizations for exposure and marketing of their practice.
Why are some networks so narrow? These networks are aiming for a truly patient centered experience. The primary care provider and the patient would make decisions together for the best course of treatment. Specialists need to decide what groups might have the biggest impact on your bottom line.
That is where the negotiating comes in. In a narrow network, the specialists need to prove their worth and may have to jump through extra hoops or make certain concessions in contract negotiations to become an in-network provider.
Is it so bad to be out of network? If you are out of network, most commercial insurance plans have an entirely separate set of benefits. Patients typically have separate (and large) deductibles and out-of-pocket maximums for out of network providers.
While the insurance company may “allow” the full fee of your service instead of a negotiated discount that an in-network provider might receive – this balance typically falls on the patient.
The patient becomes responsible for the entire balance. Large medical bills are extremely scary for patients.
Scary may not even be the correct term – if they don’t know it is coming, they can be outright mad. Collecting money from patients is typically much more difficult than collecting from an insurance company.
Why aren’t there set fee schedules which all insurance companies just pay the same [Pay transparency]? That is a discussion we all need to continuously be asking our legislators. Until the “system” changes this is the game – if you don’t play, other will. PractiSynergy understands and knows how to play this game. We guide providers in revenue cycle management to maximize their profits. This all starts with contracts and credentialing.
Want to get in the game and learn more about credentialing and contract negotiations?
Call Katie at PractiSynergy or reach out via Email to receive a FREE CONSULTATION on how PractiSynergy might help your practice maximize revenues through payer contracting and credentialing strategies.